Neck Pain
For chronic neck pain, quick fixes and immediate cures do not happen. Patients need to work with their health care team to try to eliminate the problem causing pain and to slow down the degenerative process. Patients should search for a “Head and Neck Surgeon near me” and choose the Southwest Scoliosis and Spine Institute for the best doctors.
The Doctors and Surgeons at the Southwest Scoliosis and Spine Institute are experts when it comes diagnosing the cause and treating the pain in the neck
Neck Pain
Over many years, our necks are subjected to repeated stress and minor injury. These injuries may not cause pain immediately after the injury. However, repeated injuries add up and can eventually result in degeneration of the cervical spine, causing neck pain. Most neck pain is caused by degenerative changes in the neck. The overall condition of the cervical spine usually determines how fast you recover from an injury and whether your neck pain will become a chronic problem. For chronic neck pain, a quick fix or complete cure cannot always turn out successfully.
You will need to work with your health care team to try to improve the problem causing pain and to slow down the degenerative process. The physician’s role in the treatment of neck pain is to find the main causes that need treatment right away. He or she will also try to keep your neck pain from becoming a chronic condition by teaching you how to slow down the degenerative process and prevent further injury.
Helping patients understand the causes of neck pain
- The normal anatomy of the spine and neck
- What you can expect from those treatments
- The signs and symptoms of degenerative changes in the neck
- The treatments available to you now and later
- What you can expect long-term if you have a problem with neck pain
Questions and Answers
What Causes Neck pain?
Neck pain can have various causes, including muscle strain or tension, poor posture, injury or trauma (such as whiplash), degenerative changes in the spine (such as osteoarthritis or herniated discs), nerve impingement, and underlying medical conditions (such as cervical radiculopathy or fibromyalgia). Identifying the specific cause requires a comprehensive evaluation by a healthcare professional.
How is Neck Pain Diagnosed?
The diagnosis of neck pain involves a combination of factors, including a detailed medical history, physical examination, and potentially diagnostic tests. The doctor will ask about the nature of the pain, its onset and duration, aggravating or relieving factors, and any associated symptoms. A physical examination may include assessing range of motion, muscle strength, reflexes, and specific tests to evaluate the neck and spine. Diagnostic tests such as X-rays, MRI scans, or electromyography (EMG) may be ordered if necessary to further evaluate the underlying cause.
What are the Treatment Options for Neck Pain?
Treatment for neck pain depends on the underlying cause and the severity of the symptoms. In most cases, doctors will initially recommend conservative treatments, including rest, physical therapy, exercise, pain medications, and hot or cold therapy. Other modalities such as massage, chiropractic care, acupuncture, or transcutaneous electrical nerve stimulation (TENS) may also provide relief. If conservative measures do not suffice, doctors will recommend more advanced interventions like injections (such as corticosteroids or nerve blocks) or surgical options. Our treatment plans pertain to each patient’s condition and recommendations are always made during discussions with the patient and their specific needs.
The Southwest Scoliosis and Spine Institute specializes in Neck Pain. Call us and Stop the Pain
General Anatomy of the Neck
To understand your symptoms and treatment choices, you must start with some understanding of the general anatomy of your spine and neck. This includes becoming familiar with the various parts that make up the neck. You should understand the function of these parts — how they work together. The more you know, the more you can talk with your doctors and healthcare team in words that will help them better understand your specific problem. It will also help you understand what they say about your particular problem.
To help patients understand their neck pain problem, information can help them make the decisions that will best help them prevent further injury, make the best treatment choices, and speed up the healing process.
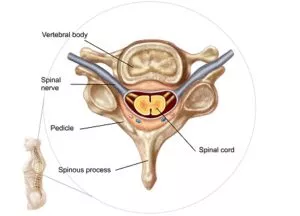
In general, the neck includes the cervical spine (the uppermost part of the spine) and the soft tissues that surround the cervical spine. These soft tissues include nerves, muscles, ligaments, tendons, and blood vessels. The cervical spine consists of the first seven vertebrae in the spine. Your doctor will usually refer to these bones as C1 through C7. The cervical spine starts just below the skull and ends just above the thoracic spine. The spine has two main functions:
- To protect and support the spinal cord
- To give structure and support to our body, allowing us to stand up straight.
The vertebrae are the 24 bones that are linked together to make up the spinal column. Just as the bones of the skull protect our brain, the bones of the spine protect the spinal cord. The spinal cord consists of a large collection of nerves that connect the brain to the rest of the body.
Vertebra
In the center of each vertebra, the doctor will see a large hole. Because the vertebrae link together, these holes line up to form a “bony tube, called the spinal canal, through which the spinal cord passes. This bony tube makes up the spinal canal, which provides protection and support for the spinal cord.
As the spinal cord leaves the brain, it travels down the spinal canal to the tailbone. Along the way, it gives off smaller nerves that leave the spine between each vertebra through an opening called the foramen. The nerves that leave the spine in the upper area, or the cervical spine, travel into the arms to the hands. The nerves that leave the spine in the chest area, or the thoracic spine, mostly go into the chest and belly area. All of the nerves that leave the spinal canal in the lower spine, or the lumbar spine, travel into the legs and feet.
Spinal Segment
To better understand how the parts of the spine work together, let’s look at a spinal segment. A spinal segment consists of two vertebrae, the intervertebral disc between the vertebrae, and the two nerve roots, one from each side, that “branch off ” the spine. The cervical vertebrae are the smallest in the spine because they do not have the weight-bearing function of the vertebrae in the back. One pair of spinal nerves exits through the gap between the vertebrae in each segment. One common cause of pain comes from pressure on the nerve roots, sometimes causing pain and numbness in the neck or the lower body.
The space between two vertebrae contains a large, round disc of connective tissue, called an intervertebral disc. By looking at the intervertebral disc from above, we can see an outer ring, called the annulus, and a soft spongy center called the nucleus pulposus. The annulus, the strongest part of the disc, helps keep the spongy center inside the disc. The nucleus pulposus acts as a shock absorber to cushion the bones from pressure during twisting, jumping, and weight-bearing.
A joint forms when two or more bones meet. Bony knobs, called facets, extend from each vertebra and overlap each other to form a facet joint. Facet joints link the vertebrae together like a chain and provide a mobile connection between each vertebra. The facet joints are important because they allow the neck to bend and turn. Each vertebra can move only a little, but the chain of small movements combined makes the spine very flexible.
The Most Common Causes of Neck Pain
The disc consists of connective tissue, which wears normally as we age. However, many of the problems that cause neck pain stem from abnormal wear and tear, poor posture, or rheumatoid arthritis. This process refers to the degeneration of the intervertebral disc. Degeneration often results from small injuries that may not cause pain at the time the injuries occur. Over time, these injuries add up, and the abnormal wear and tear can weaken the connective tissue that makes up the disc. Once the connective tissue becomes weak, sudden stress, such as a whiplash-type movement, may injure the disc more easily. The entire process of disc degeneration refers to spondylolysis of the cervical spine.
To understand neck pain, you need an understanding of the wear-and-tear process, called disc degeneration. This will also help you later understand what can happen to the neck when a sudden injury can cause immediate pain and dysfunction. The next section will explain both the process of degeneration and the most common causes of pain in the neck.
Degenerative Disc Disease
To help you understand disc degeneration, compare a spinal segment to two vanilla wafers (the “vertebrae”) and a marshmallow (the “disc”). Imagine a fresh marshmallow between the two wafers. When you press the wafers close together, the marshmallow gives or “squishes out”. Suppose you leave the marshmallow out for a week and it starts to dry out. When you press it between the wafers, it should not seem quite as spongy. If you press hard enough, the outside of the marshmallow may even tear or split. Suppose you left the marshmallow out for a month. It would probably appear so dried out that it would be hard and very thin and would not have any “shock absorbing” ability.
As we age, the disc loses some of its water content and, as a result, some of its shock-absorbing ability. Like the marshmallow, the first changes that occur in the disc are tears in the outer ring of the disc, called the annulus. Tears in the annulus may occur without symptoms. Therefore, you may not notice when they occur or what causes them. These tears heal by forming scar tissue. Scar tissue appears weaker than normal tissue. Repeated injuries and tears cause more wear and tear to the disc. As the disc wears, it loses more of its water content. It becomes less and less “spongy” and eventually no longer able to act as a shock absorber.
Disc Wear
As the disc continues to wear, it begins to collapse. The space between each vertebra becomes smaller. The collapse also affects the way that the facet joints in the back of the spine “line up”. Like any other joint in the body, the change in the way the bones fit together causes abnormal pressure on the articular cartilage. Articular cartilage appears as the smooth, shiny material that covers the ends of the bones in any joint. Over time, this abnormal pressure causes wear and tear arthritis (osteoarthritis) of the facet joints.
Bone spurs may form around the disc and facet joints. Doctors believe that too much motion in a spinal segment causes bone spurs to form. Eventually, bone spurs can form around the nerves of the spine, causing a condition called spinal stenosis.
Spinal Conditions
Degeneration of the disc and spinal segment can result in several different spinal conditions that cause problems. These include mechanical neck pain, cervical radiculopathy, and spinal stenosis. Sometimes we may injure our neck with a relatively minor injury. These minor injuries may cause pain for a few days and then go away. This refers to a neck or muscle strain. We may never fully understand what has been injured in one of these episodes. In the next section, we will try to explain each condition and how they differ.
Muscle Strain
A “muscle strain” of the neck occurs when a patient presents with a stiff neck. In some cases, this may represent a true “muscle strain” or “pulled muscle” involving the muscles around the spine of the neck. However, a muscle spasm can result when other areas of the neck are injured. Problems that doctors refer to as muscle strain may also involve injury of other soft tissues of the neck, including the disc, the ligaments around the spinal segment, and the muscles. Injury to any or all of these structures may cause similar symptoms.
Mechanical Neck Pain
A chronic neck ache where the pain stays mainly in the neck may occur as a result of degenerative disc disease and arthritis of the facet joints of the cervical spine. Doctors sometimes refer to this type of pain as mechanical pain. Doctors use this term because it gets worse when we use our neck more and seems to emanate from the parts of the cervical spine — the mechanical parts that allow us to move our head around and up and down.
This type of pain does not come from pinched or irritated nerves. The pain seems to come from the inflamed facet joints and the degenerated disc. As the disc and facet joints become more inflamed when we use our neck to move our head, the muscles around the cervical spine begin to spasm. You can think of a muscle spasm similar to a muscle cramp. Muscle cramps eventually cause pain. The spasm occurs as the body’s response to try to stop the movement in the cervical spine.
Cervical Radiculopathy (Pinched Nerve)
When a nerve root leaves the spinal cord and the cervical spine, it travels down into the arm. Along the way, each nerve supplies sensation (feeling) to a part of the skin or shoulder and arm, and supplies electrical signals to certain muscles to move part of the arm or hand. When a nerve becomes irritated or pinched by either a bone spur or part of the intervertebral disc, it causes the nerve not to work properly. This shows up as weakness in the muscles the nerve travels to; numbness in the skin where the nerve goes, or pain in the area where the nerve travels. This condition refers to cervical radiculopathy. Let’s look at the different causes of cervical radiculopathy.
Pinched Nerve from a Herniated Disc
Pressing the wafers together on one side would cause the marshmallow to bulge out on the opposite side.
 Injury to the disc may occur when neck motion puts too much pressure on the disc. Getting a herniated disc presents a lot of pain. In this injury, the tear in the annulus causes part of the nucleus pulposus to squeeze out of the center of the disc. The annulus can tear or rupture anywhere around the disc.
Injury to the disc may occur when neck motion puts too much pressure on the disc. Getting a herniated disc presents a lot of pain. In this injury, the tear in the annulus causes part of the nucleus pulposus to squeeze out of the center of the disc. The annulus can tear or rupture anywhere around the disc.
If it tears on the side next to the spinal canal, then when the nucleus pulposus squeezes out, it can press against the spinal nerves. Pressure on the nerve root from a herniated disc can cause pain, numbness, and weakness along the nerve. Evidence reveals that the chemicals released from the ruptured disc may also irritate the nerve root, leading to some of the symptoms of a herniated disc — especially pain.
Herniated discs become more common in early, middle-aged adults. This condition may occur when too much force is applied to an otherwise healthy intervertebral disc. An example would be a car accident where the driver or passenger’s head would hit the windshield. That force on the neck would exceed even a healthy disc’s ability to absorb without any injury.
A herniated disc may also occur in a disc that has been weakened by the degenerative process. Once weakened, less force will cause the disc to tear or rupture. However, not everyone with a ruptured disc possesses degenerative disc disease. Likewise, not everyone with degenerative disc disease will suffer a ruptured disc.
Pinched Nerve from Degeneration and Bone Spurs
In middle-aged and older people, degenerative disc disease can cause bone spurs to form around the nerve roots. This usually occurs inside the foramen – the opening in the cervical spine where the nerve root leaves the spine to travel into the arm. If these bone spurs get large enough, they may begin to rub on the nerve root and irritate it. This causes the same symptoms as a herniated disc. The irritation causes: pain to run down the arm, numbness to occur in the areas to which the nerve provides sensation, and weakness in the muscles that the nerve supplies.
Spinal Stenosis (Cervical Myelopathy)
Perhaps the most serious of the problems caused by degeneration of the cervical spine occurs with spinal stenosis. In the late stages of spinal degeneration, bone spurs from the degenerative process can cause a condition known as spinal stenosis. As the bone spurs form, the size of the spinal canal becomes smaller.
The bone spurs begin to press on the spinal cord or the nerve roots. Pressure on the nerves in the spinal cord can cause numbness, tingling, or pain in the arms, hands, and legs. This condition refers to cervical myelopathy and differentiates from the simpler problem where only one nerve root becomes pinched by a herniated disc or a bone spur.
When the narrowing of the spinal canal (the bony tube where the spinal cord runs) occurs, the whole spinal cord can become affected. This is different than when the bone spurs narrow one of the foramina (the openings where the nerve roots exit). The symptoms are much different. A pinched nerve from either a herniated disc or a bone spur rarely affects the legs. Cervical myelopathy can affect both the arms and the legs.
When Should I Consult a General Practitioner for Neck Pain?
Experiencing neck discomfort can be unsettling, but knowing when to seek professional advice is crucial. Here are some situations when you should consider finding a “Head and Neck Surgeon Near me”.
- Persistent Discomfort: If your neck pain lingers for several weeks without improvement, it’s advisable to consult a healthcare professional.
- Ineffective Over-the-Counter Relief: Should common pain relievers such as acetaminophen or ibuprofen offer little to no relief, it’s a good idea to seek medical advice.
- Concerns About Severity: Anytime you’re anxious about the severity or nature of your pain, it’s better to get it evaluated by a doctor.
- Accompanying Symptoms: If you notice additional symptoms like tingling, numbness, or weakness in an arm, it could indicate a more serious condition that needs medical attention.
Symptoms
Symptoms are how the cause of your pain affects you. Common symptoms include:
- Pain in your neck
- Headaches
- Pain in your shoulder, arm, or hand
- Reduced range of motion in your neck
- Numbness, weakness, and slower reflexes in your arms, hands, legs, or feet
- Problems walking, including a “spastic gait.”
- Muscle weakness in your legs
Diagnosis
Finding the cause of neck pain begins with a complete history and physical examination. After the history and physical exam, your doctor will better understand the cause of your pain. To make sure of the exact cause of your neck pain, your doctor can use several diagnostic tests. These tests will find the cause of your pain. Regular X-rays taken in the doctor’s office will begin the first step in looking into any neck problem and will help determine if more tests are needed.
Complete History
A “complete history” usually occurs in two parts. The first part gets written on a form that you fill out while you wait to see the doctor. While you fill out the form, take time to think about everything you can remember that relates to your neck pain, and write it down. The more you can tell your doctor, the faster he or she can diagnose the cause and help relieve your pain. The second part of your history consists of questions being answered. Your doctor will ask you to describe when your neck pain began and the type of pain you experience.
Questions to ask a Doctor
- When did the pain first begin?
- When did you increase your activity level?
- Have you undergone surgery on your neck?
- Does the pain go down into your arms or legs?
- What causes your neck to hurt more or less?
- Have you had any problems with your bowels or bladder?
Physical Examination
Once the doctor gets all of the information, the doctor will give you a thorough physical exam. During the exam, your doctor will look at your neck to see how it functions. This includes:
- How well you can bend your neck and roll your head in all directions
- How well you can twist your neck
- If there is tenderness around the neck
- If there are muscle spasms around the neck and shoulders
Tests that examine the nerves that leave the spine are also important. These include:
- Arms and hands testing
- Reflex testing
- Testing the strength of the muscles in the arms, hands, and legs
- Testing for signs of nerve irritation
X-rays
 X-rays show the bones of the cervical spine. Most of the soft tissue structures of the spine, such as the nerves, discs, and muscles, do not show up on X-rays. X-rays can show problems that affect the bones, such as infection, fractures, or tumors of the bones. X-rays also provide information regarding the degree of spine degeneration, but they will not show a herniated disc. Also, the narrowing of the disc space between each vertebra and bone spurs does show up on X-rays. The X-rays will show how much degeneration and arthritis are affecting the neck.
X-rays show the bones of the cervical spine. Most of the soft tissue structures of the spine, such as the nerves, discs, and muscles, do not show up on X-rays. X-rays can show problems that affect the bones, such as infection, fractures, or tumors of the bones. X-rays also provide information regarding the degree of spine degeneration, but they will not show a herniated disc. Also, the narrowing of the disc space between each vertebra and bone spurs does show up on X-rays. The X-rays will show how much degeneration and arthritis are affecting the neck.
Magnetic Resonance Imaging (MRI)
Doctors use MRI to evaluate the spine because it can show abnormal areas in the soft tissues around the spine. The MRI outperforms an X-ray because, in addition to the bones, it can also show pictures of the nerves and discs. An MRI finds tumors, herniated discs, or other soft-tissue disorders. The MRI test lasts about 90 minutes. During the MRI, very detailed computer images of sections of the spine are taken. Unlike most other tests, which use X-rays, the MRI uses magnetic fields and radio waves to see the structures of the neck. Pictures can also be taken in a cross-sectional view.
The MRI allows the doctor to see the nerves and discs without using special dyes or needles. In many cases, doctors will only use the MRI because it will find the cause of a patient’s neck pain. Before the MRI begins, you will be asked to remove any metal objects, such as jewelry. Staff will ask if you have metal implants, such as a pacemaker or joint replacement. Because of the strong magnetic field, people with certain types of metal implants cannot undergo an MRI.
The MRI scanner is a very large machine with a tunnel-like area in the center. While you lie on a table, the table slides into the tunnel of the scanner. Once in position, you will be asked to remain very still for the rest of the test. During the test, you will hear clicking and thumping noises as the scanner moves. While the scanner takes pictures, the technician can see the pictures on a monitor and record them.
Computer-Assisted Tomography (CAT Scan)
 The CAT scan, a very detailed X-ray, appears very similar to the MRI. During a CAT scan, cross-sectional X-rays, or X-ray “slices”, are taken of the spine. The CAT scan shows the bones of the spine much better than the MRI does; however, the MRI shows soft tissues better than the CT. The doctor will use a CAT scan when the doctor suspects a condition that only affects the bones of the spine. The CAT scan and a myelogram get better pictures of the spinal nerves. Together, these two tests can help determine if the pressure on the nerve comes from spinal stenosis or a herniated disc.
The CAT scan, a very detailed X-ray, appears very similar to the MRI. During a CAT scan, cross-sectional X-rays, or X-ray “slices”, are taken of the spine. The CAT scan shows the bones of the spine much better than the MRI does; however, the MRI shows soft tissues better than the CT. The doctor will use a CAT scan when the doctor suspects a condition that only affects the bones of the spine. The CAT scan and a myelogram get better pictures of the spinal nerves. Together, these two tests can help determine if the pressure on the nerve comes from spinal stenosis or a herniated disc.
The CAT scan performs much like the MRI scan and will make images while you lie very still on a table that slides into the scanner. The CAT scan lasts about 30 to 60 minutes. A contrast dye may be used for better pictures. After the pictures have been taken, you get up, dress, and leave the room.
Myelography (Myelogram)
A doctor uses Myelography to evaluate an area of the spine called the subarachnoid space. Doctors use Myelography to find herniated discs, injuries to the spinal nerve roots, or tumors. During this test, a special dye, which can be seen on the X-ray, gets injected into the spinal sac. Because the dye weighs more than the spinal fluid, the movement of the dye can be watched as the table tilts up and down. By watching the movement of the dye, the doctor can see the outline of the subarachnoid space. If the shape of the spinal sac looks abnormal or indented, this may indicate pressure on the nerves of the spine. A herniated disc may cause this pressure.
Before your test, you will have a restricted diet. The test begins with the doctor inserting a needle between two discs in your back. This occurs while you lie on the edge of the table with your chin on your chest and your knees drawn up toward your chest. Then, once the needle is in place, you will turn over and lie flat on your stomach.
After that, the nurse will strap you to the table that tilts for the test. The doctor will inject dye into your back. You may notice a brief burning and warm feeling as the dye goes into your body. As the table tilts, the dye will flow through the spinal area. The doctor will watch the flow of the dye, take X-rays, and then remove the needle. After the test, the patient will rest in the hospital for several hours or maybe overnight.
Electromyogram (EMG)
 An EMG tests the speed at which the nerve roots send electrical messages to the brain. The doctor performs the test by inserting tiny needle electrodes into the muscles of the lower leg. The EMG measures the electrical signals in the muscles. An EMG can show a pinched nerve after it branches from the spine. Before the test, you may have some restrictions on what you eat or drink, including certain medications. You will need to sign a consent form. During the test, you will lie down or sit so that the muscles being tested are at rest.
An EMG tests the speed at which the nerve roots send electrical messages to the brain. The doctor performs the test by inserting tiny needle electrodes into the muscles of the lower leg. The EMG measures the electrical signals in the muscles. An EMG can show a pinched nerve after it branches from the spine. Before the test, you may have some restrictions on what you eat or drink, including certain medications. You will need to sign a consent form. During the test, you will lie down or sit so that the muscles being tested are at rest.
Then a needle electrode gets inserted into the muscle, and you may feel some discomfort. A metal plate that records the electrical signal gets placed under you. Abnormal electrical activity can indicate a pinched nerve. The test lasts about an hour.
Bone Scan
A bone scan helps locate the affected area of the spine. To perform a bone scan, a radioactive chemical is injected into the bloodstream. The radioactive chemical attaches itself to areas of bone that are undergoing rapid changes for any reason. Areas of the skeleton that are undergoing rapid changes appear as dark areas in the film. Once the affected area is identified, other tests, such as an MRI scan, are done to look more closely at the specific area.
Laboratory Tests
There are many possible causes of neck pain. Some of these causes are not related to the degeneration of the spine. Blood tests to look for infection or arthritis may take place. Problems originating in areas other than the spine may also cause neck pain. If your doctor feels that you may have a throat problem or a thyroid problem, other tests may be ordered to identify where the problem originates.
Treatment
Treatment for any neck condition should involve two goals:
- Relieve pain
- Reduce the risk of re-injury
The diagnosis of neck pain can range from there being no problem to very delicate surgery. In general, treatment for neck pain falls into two broad categories: conservative treatment (non-surgical) and surgical treatment.
Conservative Treatment – Non-Surgical Treatment for Your Neck Pain
Medications
Medications are commonly used to control pain, inflammation, muscle spasms, and sleep disturbance. Some general tips about treatment with medication:
- Patients should take medication wisely! Take all medications exactly as prescribed and report any side effects to your doctor.
- Muscle relaxers and pain relief medications are sometimes prescribed.
- Some pain medicines are highly addictive!
- No pain medicine will control chronic pain if used over a long period.
- No medication will cure neck pain of degenerative origin.
Cervical Collar
 While an injured neck heals, a cervical collar provides support and limits motion. It also helps keep the normal alignment. Cervical collars can be soft (made of foam) or hard (made of metal or plastic). Because these collars can restrict the movement of your head, you may need help with eating and other activities. The skin under the collar needs checking every day to prevent blisters or sores.
While an injured neck heals, a cervical collar provides support and limits motion. It also helps keep the normal alignment. Cervical collars can be soft (made of foam) or hard (made of metal or plastic). Because these collars can restrict the movement of your head, you may need help with eating and other activities. The skin under the collar needs checking every day to prevent blisters or sores.
Cervical Pillow
Doctors will recommend a cervical pillow for people who have problems with neck pain at night. The cervical pillow holds the neck in the best position to prevent excess stress on the cervical spine during sleep.
Physical Therapy
Your doctor may order a physical therapist to work on an exercise program developed just for you. The physical therapist will teach you ways to prevent further injury to your neck.
Epidural Steroid Injection (Nerve Block)
If other treatments do not relieve your back pain, you may be given an epidural steroid injection (ESI) or a cervical nerve block. An ESI places a small amount of cortisone into the bony spinal canal. Cortisone may control the inflammation surrounding the nerves and may ease the pain caused by irritated nerve roots. The ESI does not always become successful. When other conservative measures do not work to postpone surgery, doctors try using this injection.
Surgical Treatment of Neck Pain
Surgery occurs for just a few people. However, no single type of surgery works for every neck pain problem. If your doctor thinks surgery will improve your neck pain, he or she will suggest the type of surgery best suited for you. Numerous surgical procedures have been designed to treat each type of neck pain. The following section describes different surgical treatments in a very general way and gives an overview of what each type of procedure tries to accomplish. Doctors recommend surgical procedures for one of three reasons:
- Removing pressure from the nerve roots caused by bone spurs or herniated disc material (for cervical radiculopathy)
- Removing pressure from the spinal cord (for cervical myelopathy)
- Stopping the motion between two vertebrae – or a spinal segment (for degenerative disc disease)
Discectomy
One of the most common surgical procedures for problems in the cervical spine is an anterior cervical discectomy. The term “discectomy” means “remove the disc”. A discectomy relieves the pressure on a nerve root by removing the herniated disc causing the pressure.
In the cervical spine, doctors usually remove a disc from the front. An incision occurs in the front of your neck, right beside your trachea (windpipe). The muscles are moved to the side. The arteries and nerves in the neck are protected as well.
Once the doctor sees the spine, each disc and vertebra are identified using an X-ray to verify the correct disc. Once verified, the doctor will remove the disc. Any bone spurs that are found sticking off the back of the vertebra are removed as well. Your surgeon will take great care not to damage the spinal cord and nerve roots.
In the cervical spine, a discectomy normally occurs with an anterior spine fusion, where the two vertebrae on either side of the removed disc heal together, or fuse. The following provides additional information on Cervical fusion.
Cervical Fusion
Once the disc has been removed between the vertebrae, a cervical fusion is performed. This procedure allows the surgeon to fill the space left by removing the disc with a block of bone taken from the pelvis. Placing a bone graft between two or more vertebrae causes the vertebrae to grow together or fuse. If your neck problem is caused by segmental instability, a spinal fusion may also be recommended – even if you do not have cervical radiculopathy
The bone graft is usually taken from the pelvis at the time of surgery, but some surgeons prefer to use a bone graft obtained from a bone bank. Bone graft from a bone bank is taken from organ donors and stored under sterile conditions until it is needed for operations such as spinal fusion. The bone goes through a rigorous testing procedure, similar to a blood transfusion. This is to reduce the risk of passing on diseases, such as AIDS or hepatitis, to the recipient.
Anterior Interbody Fusion
This type of fusion is much more common in the neck and is described above. When implementing interbody fusion, a bone graft is placed between two vertebrae and replaces the removed disc. During the healing process, the vertebrae grow together, creating a solid piece of bone out of the two vertebrae. Anterior interbody cervical fusion is used to treat most problems in the neck caused by degenerative disc disease. In addition, this procedure is used to correct unrelieved neck pain and pressure on spinal nerve roots caused by bone spurs or a herniated disc.
The goal of spinal fusion is to stop the motion caused by segmental instability. This reduces the mechanical neck pain caused by excess motion in the spinal segment. The anterior cervical fusion may also be done in a way that spreads the vertebrae apart a bit, trying to restore the space between them. Increasing the distance between the vertebrae also makes the foramen larger in the back part of the spinal column. This may reduce the pinching and irritation of the nerve roots by bone spurs around the foramen.
Posterior Fusion
You may hear the term posterior fusion as well. In the posterior fusion, the bone graft is placed on the backside of the vertebrae. During the healing process, the vertebrae grow together, creating a solid piece of bone out of the two vertebrae. This type of fusion is only rarely used in the cervical spine, generally only for fractures of the spine.
When conducting a cervical posterior fusion, the bone graft may simply get wedged in between the vertebrae. It gets held there simply because it is wedged in tight. In recent years, there has been an increase in the use of metal plates, screws, and rods to try to increase the success of helping the spine to fuse.
Many different types of metal implants are used to hold the vertebrae in position while the fusion heals. Bone heals best when it remains still, without motion between the pieces trying to heal together. The healing of a fusion appears no differently than healing a fractured bone, such as a broken arm. However, the neck is a difficult part of the body to hold still.
Laminectomy
If spinal stenosis is the main cause of your neck pain, then the spinal canal must be made larger, and any bone spurs pressing on the nerves must be removed. One way that this is done is with a complete laminectomy. Laminectomy means “remove the lamina”. Remember from the anatomy section that the lamina is the backside of the spinal canal and forms the roof over the spinal cord. Removing the lamina gives more room for the nerves and allows the removal of bone spurs that form around the nerves. A laminectomy reduces the pressure on the spinal cord and the irritation and inflammation of the spinal nerves.
In the cervical spine, removing the lamina completely may cause problems with the stability of the facet joints between each vertebra. If the joints are damaged during the laminectomy, the spine may begin to tilt forward, causing problems later. One way that spine surgeons try to prevent this problem is not to remove the lamina. Instead, they simply cut one side of the lamina and fold it back slightly. The other side of the lamina opens like a hinge. This makes the spinal canal larger, giving the spinal cord more room. The cut area of the lamina eventually heals to keep the spine from tilting forward.
Corpectomy and Strut Graft
Perhaps a more popular procedure for removing the pressure on the spinal cord causing spinal stenosis and cervical myelopathy is to remove the front of the spinal canal. This means the removal of a large part of several of the vertebrae – the vertebral bodies and the discs between. This procedure is called a corpectomy. “Corpus” means body, and “ectomy” means to remove. Once the vertebral bodies are surgically removed, the space must be filled with something.
Again, just as in the anterior cervical fusion, this space normally gets filled with a bone graft. Some type of internal fixation is usually required to hold the vertebrae and the bone graft in place. You will probably also need to be placed in a halo jacket to hold your head perfectly still while the healing occurs and the vertebrae fuse. This is a very uncommon procedure.
Learn more about the Corpectomy and Strut Graft
Learn more about the use of bone grafts.
Surgical Complications
With any surgery, there is a risk of complications. When surgery is done near the spine and spinal cord, these complications (if they occur) can be very serious. Complications could involve subsequent pain and impairment and the need for additional surgery. You should discuss the complications associated with surgery with your doctor before surgery. The list of complications provided here is not intended to be a complete list of complications and is not a substitute for discussing the risks of surgery with your doctor. Only your doctor can evaluate your condition and inform you of the risks of any medical treatment he or she may recommend.
Anesthesia
Any operation that requires some type of anesthesia can be potentially harmful. Surgery on the cervical spine usually requires that you be put under general anesthesia. General anesthesia means that you are put to sleep. Anesthesia carries a risk of allergies to the medications. Different life-threatening situations can occur during anesthesia. It is extremely unlikely that these complications will occur, but you should be aware that they are possible.
Infection
Any surgery involving an incision in the skin can become infected. In addition, the bone graft and area around the spine may become infected. An infection will usually require some type of antibiotic medication to treat the infection. If the infection involves the bone, it may require one or more additional operations to drain the infection. The risk of infection is probably less than one percent.
Blood Vessel Damage
Some large arteries and veins travel through the neck into the brain. The carotid artery and the jugular vein are nearby. It is possible to damage these blood vessels during the surgery. It is extremely unlikely that this will occur, probably less than one in a thousand.
Nerve Damage
There are nerves in the neck that travel along the area where the incision is made to perform an anterior cervical discectomy and fusion. These nerves go to the vocal cords. There is a possibility that these nerves can be damaged during surgery. This can lead to hoarseness. If this occurs, it will usually recover unless the nerve is permanently damaged or cut. Again, this is unlikely.
Spinal Cord Damage
Operations that are performed on the cervical spine out of necessity place the spinal cord at risk for injury. Spinal cord damage is probably much more likely in larger, more serious operations such as corpectomy and strut grafting procedures. These are complex, difficult operations and are done for extremely serious problems that are unlikely to respond to any other type of treatment.
The routine anterior discectomy and fusion is a common operation that is extremely safe. While damage to the spinal cord is possible, it is highly unlikely.
Graft Displacement
One of the more common problems that can occur after an anterior cervical discectomy and fusion is that the bone graft may move out of position. Thus, if it moves too much, it may require a second operation to place a new bone graft in its place.
Despite a successful operation and good bone graft, a fusion may not occur between the vertebrae. This is termed a non-union. Usually, your surgeon will be able to tell if a fusion has occurred by looking at X-rays taken over a three to six-month period following the surgery. If a fusion does not occur and you have no pain, a second operation will not be necessary. If you continue to have pain and a non-union is diagnosed after surgery, your surgeon may suggest a second attempt at fusion. When trying for the second time after a failed fusion, most surgeons will usually include some type of internal fixation, such as a plate and screws.
Rehabilitation
Your doctor may have you see a physical therapist who will design a neck-care program just for you. This program may include neck flexibility exercises to specifically target stiffness and improve your range of motion. These exercises can be simple yet effective, such as gentle neck tilts and rotations, which you can perform daily to maintain flexibility.
Also, your physical therapist will evaluate your condition and design a program to ease your pain and help your neck move better. They may suggest a variety of exercises, including:
- Chin tucks to strengthen neck muscles
- Neck stretches to relieve tension
- Isometric exercises to improve stability
Finally, your doctor will provide methods to take care of your neck so you can avoid pain and prevent further injury to your neck. This may include ergonomic tips for your workspace, advice on maintaining good posture, and strategies for managing stress, all of which contribute to overall neck health.
In addition to professional guidance, there are several measures you can take yourself to manage neck pain effectively:
Self-Care Tips for Easing Neck Pain
Do
- Take over-the-counter pain relief: Consider medications like paracetamol or ibuprofen, or apply ibuprofen gel directly to the neck.
- Use appropriate bedding: Opt for a low, firm pillow to support your neck while sleeping.
- Apply heat or cold therapy: Alternate between applying a pack of frozen peas wrapped in a tea towel for 5 minutes, 3 times a day, and a hot water bottle wrapped in a tea towel for 20 minutes, 2 to 3 times daily.
- Practice neck flexibility exercises: Gentle stretches and movements can enhance neck mobility and reduce discomfort.
Don’t
- Avoid neck collars: Unless specifically advised by a doctor, keep your neck moving to promote healing.
- Steer clear of risky activities: If restricted neck movement is a concern, avoid tasks like driving or cycling that require a full range of motion.
By combining these self-care practices with the expertise of your physical therapist, you can address neck pain effectively while minimizing the risk of further injury.
The Expertise a Doctor Needs to Diagnose and Treat Pain in the Neck
Remember, finding the right doctor or “neck and shoulder doctor near me” is a personal decision, and it’s important to find someone with whom you feel comfortable and confident. Seeking recommendations from trusted sources, researching the doctor’s credentials and experience, and scheduling an initial consultation can help you assess if they possess the knowledge, skills, and abilities necessary to diagnose and treat your neck pain effectively.
To locate neck pain treatment services in your area, consider taking these steps:
- Consult Your Local Health Clinic: Speak with the reception staff about available services, or explore their website for more information.
- Reach Out to Your Healthcare Network: Contact your integrated care board or equivalent in your region to discover local options.
- Conduct an Online Search: Use search engines to look for treatment centers or specialists nearby by typing in keywords like ‘neck pain treatment near me.’
By combining these practical steps with your personal preferences and comfort level, you can efficiently find a healthcare provider who meets both your medical needs and personal criteria.”
When seeking a doctor to diagnose and treat neck pain, it is essential to consider the many different facets of their practice. Here are some key factors to look for, which the doctors, surgeons, and staff possess at the Southwest Scoliosis and Spine Institute:
Knowledge
- Expertise: Our doctors specialize in musculoskeletal or orthopedic medicine and pain management. We have in-depth knowledge of the anatomy, physiology, and pathologies related to the neck and spine.
- Current Research: Our doctors stay updated with the latest research, treatment modalities, and evidence-based practices in the field of neck pain management.
- Diagnostic Skills: Our doctors possess a strong foundation in diagnostic skills, including history-taking, physical examination, and ordering and interpreting relevant diagnostic tests (such as imaging studies or electromyography) to identify the underlying cause of neck pain accurately.
Skills
- Comprehensive Evaluation: Our skilled doctors will perform a thorough evaluation of your neck pain, taking into account factors such as medical history, lifestyle, occupational factors, and any previous treatments.
- Physical Examination: The Doctors at the Southwest Scoliosis and Spine Institute possess proficient hands-on skills to assess the range of motion, muscle strength, sensation, and specific neck and spine tests to identify potential structural abnormalities or musculoskeletal imbalances.
- Treatment Modalities: Our Doctors are skilled in a wide range of treatment modalities, including conservative approaches (such as physical therapy, exercise programs, and medications) as well as more advanced interventions (such as injections or minimally invasive procedures) if necessary. When dealing with neck pain, understanding your medication options is crucial. Over-the-counter solutions such as:
- Paracetamol: Often recommended for its effective pain-relieving properties.
- Ibuprofen: Known for reducing inflammation and pain, available orally or as a topical gel for targeted relief.
These medications can offer significant relief and are generally safe for short-term use. It’s always advisable to consult with a healthcare professional if pain persists, to explore further treatment possibilities tailored to your specific needs.
Abilities
- Effective Communication: The Doctors at the Southwest Scoliosis and Spine Institute possess excellent communication skills, actively listening to your concerns, explaining complex medical terms in understandable language, and ensuring you have a clear understanding of the diagnosis and treatment plan.
- Patient-Centered Care: Our doctors take into account a patient’s preferences, goals, and limitations when formulating a treatment plan. They involve their patients in decision-making and address any questions or concerns they may have.
- Holistic Approach:
Neck pain can have multiple contributing factors, including physical, psychological, and lifestyle-related aspects. Our doctors will consider the whole person and adopt a holistic approach to treatment, addressing not only the physical symptoms but also factors such as stress management, ergonomics, and lifestyle modifications.
To effectively prevent neck pain, consider the following practical tips:
Sleeping Tips
- Ensure your head is aligned with your body, using a pillow that maintains this height.
- Opt for a firm mattress to support your spine properly.
- Avoid sleeping on your front, which can strain your neck.
Posture and Movement
- Sit upright, gently rolling your shoulders back and aligning your neck.
- Avoid keeping your neck in a fixed position for extended periods, such as when working at a desk.
- Refrain from twisting your neck when lying in bed.
By integrating these preventive measures with our holistic treatment, you can address both the immediate discomfort and the underlying factors contributing to neck pain. This comprehensive approach not only alleviates current symptoms but also promotes long-term well-being.
____________________
Citation: HealthLine: Neck Pain
The medical content on this page has been carefully reviewed. It was approved for accuracy by the Southwest Scoliosis and Spine Institute’s qualified healthcare professionals. This includes our board-certified physicians and Physician Assistants. Our team ensures that all information reflects the latest evidence-based practices and meets rigorous standards of medical accuracy, with oversight from our expert spine doctors to guarantee the reliability of our information for our patients.
If you or a loved one suffers from spinal pain, you owe it to yourself to call Southwest Scoliosis and Spine Institute at 214-556-0555 to make an appointment.