OSTEOPOROSIS
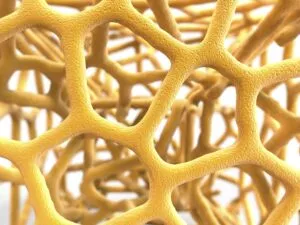
Osteoporosis is a bone disease that occurs when the body loses bone density, makes too little bone, or both. As a result, bones become weak and may break from a fall or, in serious cases, from sneezing or minor bumps. Osteoporosis means “porous bone.” Viewed under a microscope, healthy bone looks like a honeycomb.
Osteoporosis
 When people get old, particularly women, bone health becomes more important. With age, there often comes a loss of height and weight, and the development of a stooped posture. For instance, a bone-thinning disease called osteoporosis often causes these body changes. Consequently, this disease is recognized by the loss of bone mass and structural deterioration of bone tissue. This leads to bone fragility and high susceptibility to spine, hip, and wrist fractures.
When people get old, particularly women, bone health becomes more important. With age, there often comes a loss of height and weight, and the development of a stooped posture. For instance, a bone-thinning disease called osteoporosis often causes these body changes. Consequently, this disease is recognized by the loss of bone mass and structural deterioration of bone tissue. This leads to bone fragility and high susceptibility to spine, hip, and wrist fractures.
Spinal fractures are the most common type of osteoporotic fracture. 40% of all women will have at least one by the time they are 80 years old. To clarify, these vertebral fractures can permanently alter the shape and strength of the spine. Most women are likely to feel some effects of osteoporosis in their lifetime!
But the good news is that you can do a lot of things to reduce and prevent loss of bone mass and fractures. New treatments for this disease are discovered each year. You can actively work to decrease your chances of suffering osteoporosis effects. The key is prevention and intervention.
Learn more about osteoporosis including:
- What causes the condition?
- What factors contribute to developing osteoporosis?
- How to diagnose the condition.
- What symptoms are present?
- What treatment options are available?
Questions and Answers
What are the Treatment Options for Osteoporosis?
Treatment for osteoporosis typically involves a combination of lifestyle modifications, medications, and dietary changes. Weight-bearing exercises, such as walking or weightlifting, can help improve bone density. Doctors will recommend Calcium and vitamin D supplementation. Also, doctors may prescribe medications like bisphosphonates, hormone therapy, or selective estrogen receptor modulators (SERMs) to slow bone loss or stimulate new bone growth.
How do Doctors Diagnose Osteoporosis?
Doctors can diagnose osteoporosis through a bone mineral density (BMD) test, commonly performed using a dual-energy X-ray absorptiometry (DXA) scan. This test measures the density of bones, typically focusing on the hip and spine. Doctors compute a T-score, which compares the individual’s bone density to that of a healthy young adult, providing an indication of osteoporosis or low bone mass.
What is Osteoporosis?
Osteoporosis is a bone disease characterized by decreased bone density and increased fragility, making bones more prone to fractures. It often occurs as a result of aging, hormonal changes (such as menopause), or certain medical conditions.
Osteoporosis Causes
Loss of bone mass begins at around age 30. Although osteoporosis might affect men, the typical sufferers are older women, particularly those who are past menopause. Bone loss becomes worse in women after menopause. This is due to the body’s lack of estrogen. When bones lose mass, they tend to weaken and become fragile. This increases the risk of fracture under stress or because of a fall-particularly in the spine and hip.
Certainly, falls in elderly women are often the result rather than the cause of hip fractures. In other words, a fragile hip bone may simply fracture and cause a person to fall. In severe cases of osteoporosis, the bones can fracture with any kind of slight movement. And this will leave some patients bedridden.
Doctors classify osteoporosis as primary and secondary. Primary osteoporosis is further divided into “primary type I” and “primary type II” osteoporosis.
Prevention
Share your family history with your physician. Let him/her know the conditions that run in your family and become aware of the risk factors. Oftentimes, people with osteoporosis don’t know they have the condition until they experience a broken bone.
According to the National Osteoporosis Foundation:
- Make sure to get enough exercise, including weight-bearing exercise.
- Include fruits, vegetables, calcium, and vitamin D in your daily diet.
- Avoid caffeine and limit alcohol.
Types of Osteoporosis
Most people think of Primary (Type I) Osteoporosis when talking about osteoporosis. It’s the form that mainly affects women after menopause. Primary type I osteoporosis is six times more common in women than men, occurring in women 15 to 20 years after menopause. The loss of bone is connected to an estrogen deficiency in women and a testosterone deficiency in men. These hormones tend to become deficient with age.
Primary (Type I)
Type I osteoporosis is sometimes called high-turnover osteoporosis. It causes a rapid loss of the spongy inner part of the bones (called trabecular bone). Normally, there is a large amount of trabecular bone in the vertebral bodies of the spine and at the end of the long bones, like the wrist. People who lose trabecular bone have a higher risk of spine and wrist fractures.
Primary (Type II) Osteoporosis
Type II osteoporosis is only two times more common in women than men. It typically occurs once people reach their 70s and 80s. Also, it is taken as the result of a deficiency in dietary calcium, age-related Vitamin D decline, or increased activity of the parathyroid glands (secondary hyperparathyroidism).
With primary type II osteoporosis, there is a simultaneous loss of both the outer bone and the spongy tissue inside the bone. Because the rate of bone turnover is much lower, primary type II osteoporosis is also called low-turnover osteoporosis. Hip fractures are the most common result of this type of osteoporosis.
Secondary Osteoporosis
This form of osteoporosis develops when another problem in the body increases the rate of bone remodeling, leading to a loss of bone mass. Majorly, two functions cause bone turnover: (1) the production of new bone, and (2) the loss (resorption) of old bone.
Subsequently, the amount of bone mass you have depends on the balance between these functions. This is your bone turnover rate. If bone production is less than the amount of resorbed bone, then there is a high risk of developing osteoporosis.
Secondary osteoporosis can occur from an imbalance in hormones:
- Hyperparathyroidism is the increased activity of the parathyroid glands.
- Hyperthyroidism is an excessive secretion of the thyroid glands.
- Diabetes is a disease where the body does not produce or use insulin correctly. This leads to hyperglycemia. This means an increase in blood sugar, increasing susceptibility to infection, and to glycosuria-glucose in the urine.
- Hypercortisolism is a result of systemic illness or long-term use of oral corticosteroids.
Secondary osteoporosis can also occur from disorders where the bone marrow cavity expands at the expense of the trabecular bone. The trabecular bones have a honeycomb appearance and large marrow spaces. If a trabecular bone is affected by increased bone marrow cavities, then it loses some of its strength.
Other Causes of Secondary Osteoporosis
- Thalassemia is a hereditary form of anemia (a problem where there are too few red blood cells).
- Multiple myeloma is a condition where there are multiple tumors within the bone and bone marrow.
- Leukemia is a serious disease that is characterized by the unrestrained growth of white blood cells in the tissues.
- Metastatic bone disease is a condition that occurs when malignant tumor cells spread from one part of the body to another. The disease travels through the blood and settles in the bones.
Risk Factors
Osteoporosis does not affect everyone. There are risk factors that may predict your chances of developing it. Some risk factors are genetic. This means you inherit them from your biological parents.
While, some risks are due to medical conditions that you may not be able to avoid, such as the use of particular medications. Risk factors that are considered “lifestyle-related” are the ones that you have the most opportunity to impact.
Symptoms
Perhaps the most common symptoms of osteoporosis are fractures. Particularly, vertebral compression fractures and hip fractures. The compression fractures in the spine caused due to weakened vertebrae can lead to pain in the mid-back. These fractures often stabilize by themselves. The pain eventually goes away. However, if the crushed bone continues to move around and break, then the pain might persist.
In severe cases of osteoporosis, actions as simple as bending forward can cause a “crush fracture” in a vertebra. This type of vertebral fracture causes loss of body height and a humped back, especially in elderly women. This disorder (called kyphosis) is an exaggeration of the curve of the mid-back. It causes the shoulders to slump forward and the top of the back to look enlarged and humped.
Consult your doctor if you have symptoms of osteoporosis. Older women should discuss their risks with their physicians. Even if they are not currently showing any signs of osteoporosis. All women should be aware of the many preventive steps. This can lower their risk of developing osteoporosis.
Diagnosis
Diagnosis generally begins with a physical exam that measures height, weight, and arm span. This gives a rough estimate of what your original height might have been in young adult life. Moreover, it will also check your posture and vertebral tenderness.
Also, your doctor may ask you to have a bone mineral density test. Bone densitometry measures the density of your bone mass. This test is not part of routine screening. But if the doctor suspects osteoporosis or you fall under the high-risk category, then this test is essential. The test uses an X-ray beam to analyze bone density.
In addition, the results are placed on a graph. T-score shows how your bone density compares to the density of a healthy person who is 30 years old. Normal bone is between 0 and 1. Bones with T-scores between 1 and 2.5 are called osteopenic, meaning “too little bone.” A T-score that is more than 2.5 below ideal levels indicates osteoporosis.
Doctors also compare your scores to people of the same age and sex. This is called a Z-score.
Those at Risk
People at risk for osteoporosis can benefit from getting this test done earlier. The results can help identify if a problem exists so proper treatment can begin sooner.
Lab tests are conducted to rule out any secondary disorders that might cause osteoporosis. Tests of urine and serum are used to look for concentrations of calcium, serum protein, inorganic phosphorus, alkaline phosphates, or complete blood cell count (CBC). The medical team can use a CBC with a separate white cell count to rule out other diseases.
Also, doctors need to consider biochemical measures of bone turnover and other clinical information. Elderly people should have thyroid function tests, serum, and urinary protein electrophoresis to rule out hyperthyroidism and multiple myeloma.
If your doctor suspects a fracture, then it is essential to take an X-ray. An X-ray can also show if there are problems with bone content. An X-ray may detect problems with osteoporosis if the bones have lost 40 percent or more of their normal substance.
Treatment Options
There is still no cure for osteoporosis. But in recent years, experts have discovered many effective treatments and prevention plans. The best treatment for osteoporosis continues to be prevention.
Physical Therapy
Your doctor may have you work with a physical therapist. A well-rounded rehabilitation program assists in calming pain and inflammation. Finally, this helps in improving your mobility and strength. And, this will help you to do your daily activities with greater ease and ability.
Physical therapists design treatment programs to improve flexibility, strength, and posture. They choose exercises to help you stabilize the spine while preventing bent positions of the spine. Therapists evaluate your balance and strength to make sure you are not at risk of having a fall. Also, they might schedule the therapy sessions 2-3 times each week for at least six weeks.
The goals of physical therapy are to help you:
- Learn correct posture and body movements to counteract the effects of osteoporosis
- Perform a routine of safe weight-bearing and resistance exercise
- Use safe lifting practices to avoid straining the spine
- Improve balance to prevent falling down
- Learn ways to manage your condition
The Southwest Scoliosis and Spine Institute
Orthopedics is a specialty of our doctors and surgeons at Southwest Scoliosis and Spine Institute. They understand your concerns, can answer your questions regarding your condition, and know how to use their specialized knowledge to assist you. Richard Hostin, MD, Devesh Ramnath, MD, Ishaq Syed, MD, Shyam Kishan, MD, and Kathryn Wiesman, MD, have many years of training and experience in Spine and Back Pain for kids, adolescents, young adults, and seniors, and can help people of all ages get back to living the life they love.
The following are just a few of the many reasons why patients choose the Southwest Scoliosis and Spine Institute.
- Spine treatment: Although we do not treat Osteoporosis, this disease causes all sorts of spine problems that we do treat
- Expertise in the spine: The team of specialists at Southwest Scoliosis and Spine Institute is spine experts. They specialize in the diagnosis and treatment of spinal conditions, ensuring the best possible care for their patients.
- Cutting-edge technology: Our practice uses the latest technology and techniques to diagnose and treat a wide range of conditions. In addition, we use minimally invasive procedures that reduce pain and promote faster recovery.
- Comprehensive care: Our practice offers a full range of services, from diagnostic imaging and physical therapy to surgery. We ensure that patients receive complete, seamless care for their spinal conditions.
- Dedicated facilities: Southwest Scoliosis and Spine Institute is dedicated to providing patients with a safe and comfortable environment.
Finally, our board-certified physicians and fellowship-trained orthopedic surgeons use the full range of treatments to treat their spine patients. Southwest Scoliosis and Spine Institute’s experts with offices in Dallas, Plano, and Frisco, Texas offer cutting-edge technology, comprehensive care, and dedicated facilities to ensure the best possible care for their patients. Get in touch with us today at (214) 556-0555 to schedule an appointment.
____________________
Osteoporosis
Listen as Dr. Richard Hostin explains how he and his team utilizes a DEXA Scan to provide an indicator of the conditions of patient’s bone quality before surgery. A patient’s bones need to be strong enough to hold spinal implants when they are required to help stabilize a patient’s spine. This is one of the tools he uses to ensure that his patients will have a successful spine surgery.
If you or a loved one suffers from spinal pain, you owe it to yourself to call Southwest Scoliosis and Spine Institute at 214-556-0555 to make an appointment.